Single-cell and spatial transcriptomics uncover the role of B cells in central nervous system pathology
Spatial Transcriptomics in CNS Analysis
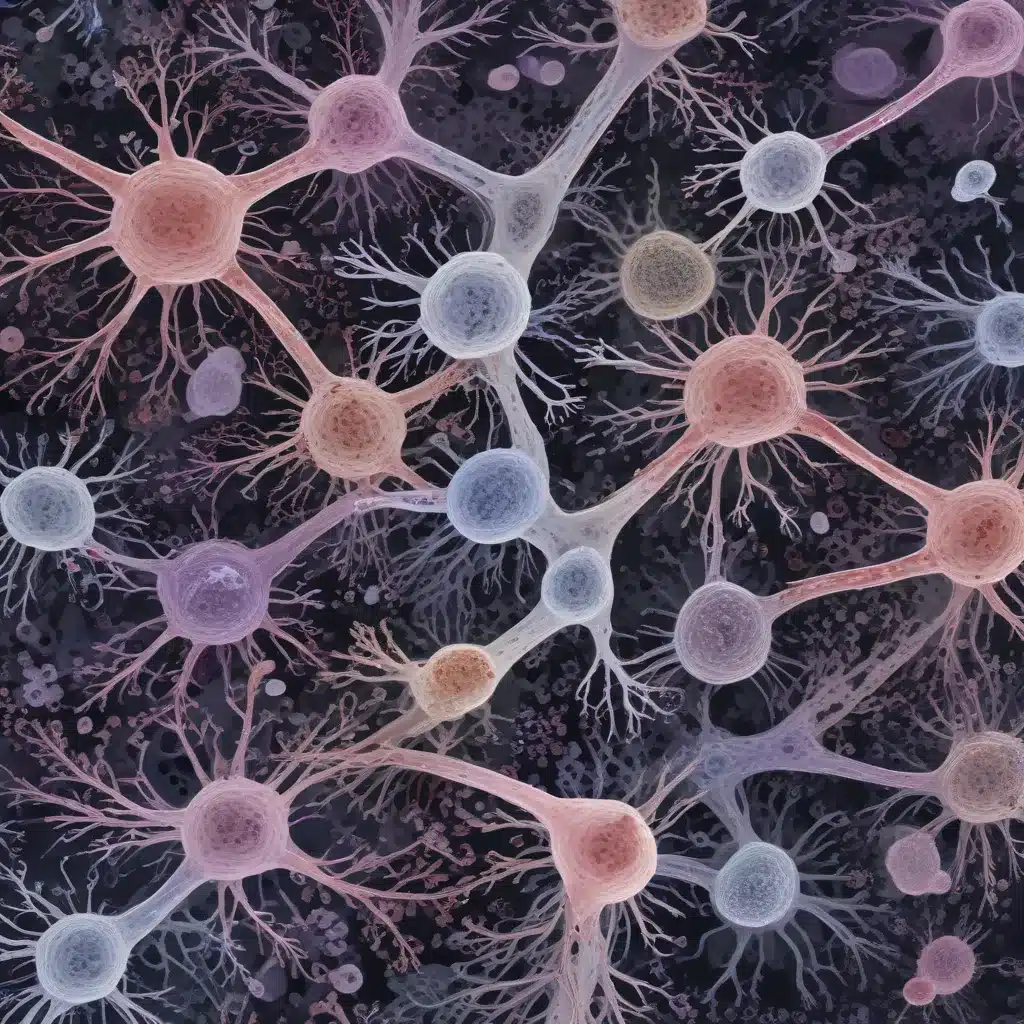
Spatial transcriptomics has emerged as a powerful technique to study the cellular complexity and spatial organization of the central nervous system (CNS) in health and disease. By preserving the spatial relationships between cells, spatial transcriptomics allows researchers to map gene expression patterns and cellular interactions within the intricate architecture of the brain and spinal cord. This approach has provided novel insights into the pathological mechanisms underlying a range of CNS disorders, from neurodegeneration to neuroimmune dysfunction.
In the study of neurological diseases, spatial transcriptomics has enabled the identification of regionally-specific alterations in gene expression that correlate with the spatial distribution of pathological hallmarks. For example, in Alzheimer’s disease, spatial transcriptomics has revealed the transcriptional changes associated with amyloid-β plaque formation, highlighting the differential responses of glial cells, such as microglia and astrocytes, in the vicinity of these lesions. This technique has also been instrumental in mapping the spatial dynamics of immune cell infiltration and activation in conditions like multiple sclerosis and amyotrophic lateral sclerosis, providing a deeper understanding of the tissue-level neuroinflammatory processes.
Single-Cell Transcriptomics in CNS Pathology
While spatial transcriptomics captures the tissue-wide context, single-cell RNA sequencing (scRNA-seq) offers a complementary approach to dissect the cellular heterogeneity within the CNS. scRNA-seq has revolutionized our understanding of the molecular diversity of neural and glial cell types, as well as their pathological changes in various neurological disorders.
In Alzheimer’s disease, scRNA-seq has revealed distinct subpopulations of microglia and astrocytes that are associated with disease progression, providing insights into their roles in neuroinflammation and neurodegeneration. Similarly, scRNA-seq studies in Parkinson’s disease have identified disease-specific alterations in dopaminergic neurons and neighboring cell types, shedding light on the selective vulnerability of these neurons.
Moreover, scRNA-seq has been instrumental in uncovering the involvement of non-neuronal cell types, such as oligodendrocytes, pericytes, and immune cells, in the pathogenesis of CNS disorders. For instance, scRNA-seq analyses have highlighted the dynamic changes in microglia and infiltrating peripheral immune cells during the course of neuroinflammatory conditions like multiple sclerosis and traumatic brain injury.
Immune Cell Dynamics in CNS Disorders
The CNS was long considered an “immune-privileged” site, but it is now well-established that immune cells play a crucial role in the initiation, progression, and potential resolution of various neurological diseases. Both innate and adaptive immune cells, including microglia, astrocytes, and T and B lymphocytes, have been implicated in the complex interplay between the brain, the immune system, and the environment.
Microglia, the resident immune cells of the CNS, have been a particular focus of attention in neurological research. scRNA-seq studies have revealed the remarkable heterogeneity of microglial responses, identifying distinct subpopulations that may be associated with neuroprotective or neurotoxic functions. Spatial transcriptomics has further elucidated the spatial distribution and interactions of microglia with other cell types, such as astrocytes and infiltrating peripheral immune cells, within the diseased CNS.
While the role of T cells in CNS disorders has been extensively studied, the involvement of B cells has remained relatively underexplored until recently. Emerging evidence from scRNA-seq and spatial transcriptomics indicates that B cells, including antibody-producing plasma cells, can infiltrate the CNS and contribute to the pathological processes in various neurological conditions.
Role of B Cells in CNS Diseases
B Cell Infiltration in Neurological Conditions
B cells have been detected in the CNS of patients with multiple sclerosis, Alzheimer’s disease, Parkinson’s disease, and other neuroinflammatory or neurodegenerative disorders. scRNA-seq studies have revealed the presence of clonally-expanded B cells and plasma cells within the brain and cerebrospinal fluid of these patients, suggesting an antigen-driven immune response.
Spatial transcriptomics has further elucidated the spatial distribution and organization of B cells in the diseased CNS. In multiple sclerosis, for example, B cells and plasma cells have been found to accumulate in ectopic lymphoid structures within the meninges, where they may contribute to the ongoing inflammation and tissue damage.
B Cell-Mediated Neuroinflammation
B cells can contribute to neuroinflammation through various mechanisms, including the production of pro-inflammatory cytokines, the presentation of antigens to T cells, and the secretion of pathogenic autoantibodies. scRNA-seq studies have revealed transcriptional profiles of CNS-infiltrating B cells that are indicative of an activated, antigen-experienced phenotype, with upregulation of genes involved in B cell receptor signaling, plasma cell differentiation, and cytokine production.
Spatial transcriptomics has provided insights into the interactions between B cells and other immune cell types within the CNS. For instance, in Alzheimer’s disease, B cells have been shown to closely interact with microglia, potentially modulating their phagocytic and inflammatory responses to amyloid-β.
Humoral Immunity and CNS Pathogenesis
Beyond their direct inflammatory effects, B cells and their secreted antibodies may also contribute to CNS pathology through more indirect mechanisms. scRNA-seq and spatial transcriptomics studies have identified the presence of autoantibodies targeting various neural antigens, including myelin proteins, neurotransmitter receptors, and synaptic proteins, in the cerebrospinal fluid and brain tissue of patients with neurological disorders.
These autoantibodies can potentially disrupt neural function, induce complement-mediated cytotoxicity, and trigger antibody-dependent cellular cytotoxicity, ultimately contributing to neuronal damage and dysfunction. Spatial transcriptomics has been instrumental in mapping the spatial distribution of these autoantibodies and their interactions with different cell types within the CNS, providing insights into their potential pathogenic mechanisms.
Emerging Techniques for CNS Immune Profiling
Integrated Omics Approaches
While scRNA-seq and spatial transcriptomics have greatly expanded our understanding of cellular diversity and spatial organization in the CNS, the integration of these technologies with other omics approaches, such as proteomics, metabolomics, and epigenomics, can provide a more comprehensive understanding of the molecular mechanisms underlying neurological diseases.
For example, the combined use of scRNA-seq and spatial metabolomics can elucidate the metabolic alterations in specific cell types and their spatial relationships within the diseased CNS, potentially identifying metabolic vulnerabilities that could be targeted therapeutically.
Computational Modeling of CNS Immunity
The wealth of data generated by scRNA-seq and spatial transcriptomics has enabled the development of sophisticated computational models to simulate and predict the complex dynamics of immune responses in the CNS. These models can integrate multi-modal data, including spatial information, to better understand the interactions between different cell types and their contributions to disease progression.
By incorporating machine learning and artificial intelligence techniques, these computational models can also be used to identify novel biomarkers and therapeutic targets, as well as to simulate the effects of potential interventions on the CNS immune landscape.
Longitudinal Tracking of CNS Immune Responses
Studying the temporal dynamics of immune responses in the CNS is crucial for understanding disease pathogenesis and informing targeted therapeutic strategies. Combining scRNA-seq and spatial transcriptomics with longitudinal sampling can provide insights into the evolving immune landscapes during the course of neurological disorders, revealing key transition points and potential therapeutic windows.
This approach can also help elucidate the role of B cells and other immune cell types in the initiation, progression, and potential resolution of CNS pathologies, paving the way for more personalized and effective therapeutic interventions.
Implications for Therapeutic Targeting of B Cells
Modulation of B Cell Function in CNS Disorders
Given the emerging evidence for the involvement of B cells in the pathogenesis of various CNS disorders, targeting B cell-mediated processes has become an area of increasing interest in the development of novel therapies. Strategies such as B cell depletion, inhibition of B cell activation and differentiation, and modulation of B cell-T cell interactions are currently being explored in the treatment of neurological conditions.
The integration of scRNA-seq and spatial transcriptomics data can help identify specific B cell subpopulations and their associated molecular signatures, guiding the development of more targeted and personalized B cell-directed therapies.
Antibody-Based Interventions in CNS Pathology
In addition to modulating B cell function, the identification of pathogenic autoantibodies through scRNA-seq and spatial transcriptomics can also lead to the development of novel antibody-based therapies for CNS disorders. These could include the use of monoclonal antibodies to neutralize specific autoantibodies or to block their interactions with target antigens in the CNS.
Spatial transcriptomics can further inform the design of these antibody-based therapies by providing insights into the spatial distribution and localization of the targeted antigens, enabling more efficient delivery and better targeting of the diseased tissue.
Combination Therapies Involving B Cell Regulation
Given the complex and multifaceted nature of CNS disorders, a combination of therapeutic strategies targeting various aspects of the immune response, including B cells, may be more effective than targeting a single pathway. scRNA-seq and spatial transcriptomics can help identify potential synergies between B cell-targeted therapies and other interventions, such as those targeting T cells, microglia, or neuroinflammatory pathways.
By elucidating the spatial and functional relationships between B cells and other cell types within the diseased CNS, these technologies can guide the development of combinatorial approaches that aim to restore the delicate balance of the immune system and promote tissue repair and regeneration.
The integration of single-cell and spatial transcriptomics has revolutionized our understanding of the cellular and molecular complexities underlying central nervous system pathologies. These powerful techniques have highlighted the critical role of B cells in the initiation, progression, and potential resolution of various neurological disorders, providing a roadmap for the development of more targeted and personalized therapeutic strategies. As the field of CNS immunology continues to evolve, the continued application and refinement of these multi-omics approaches will undoubtedly lead to further breakthroughs in our understanding and treatment of neurological diseases.